

Maintenance of wakefulness test (MWT) performed during the therapy with modafinil 400 mg/day and clomipramine 50 mg/day showed that the treatment effectiveness was insufficient (mSL 10.8 minutes). In 2005, treatment with modafinil and clomipramine was initiated. NT1 was therefore diagnosed according to the criteria of the International Classification of Sleep Disorders – 3rd edition. He tested positive for the narcolepsy associated human leukocyte antigen (HLA) DQB1*06:02 allele, and the orexin level detected with radioimmunological assay in cerebrospinal fluid (CSF) was decreased (<100 pg/mL). Urine toxicology screening was not performed. Multiple sleep latency test (MSLT) showed a mean sleep latency (mSL) of 8 minutes: sleep latency, respectively, of 7.5, 5.5, 14, 3.5 and 8.5 minutes for each test, with two sleep-onset on REM sleep periods (SOREMP) during the fourth (REM sleep latency of 10.5 minutes) and fifth (REM sleep latency of 1 minute) naps. The overnight video-polysomnography (v-PSG) revealed the following: total sleep time (TST) of 476 minutes sleep onset latency of 4 minutes rapid eye movement (REM) sleep latency of 96 minutes wake time after sleep onset (WASO) of 70 minutes arousal and awakening index of 20/hour mild obstructive sleep apnea syndrome (OSAS) with an apnea–hypopnea index (AHI) of 8/hour and a periodic limb movement (PLM) during sleep index of 24/hour (including 5/hour that were associated with micro-arousals). Baseline sleep tests were recorded without any ongoing medications. On the first presentation at a sleep center, a few months after the symptoms onset, the Epworth Sleepiness Scale (ESS) score was 19. Furthermore, clinical data did not support a diagnosis of circadian rhythm sleep-wake disorder, sleep deprivation or mood disorder. There was no personal history of head trauma or family history of narcolepsy. He did not mention the occurrence of sleep paralysis, sleep hallucinations or parasomnias.
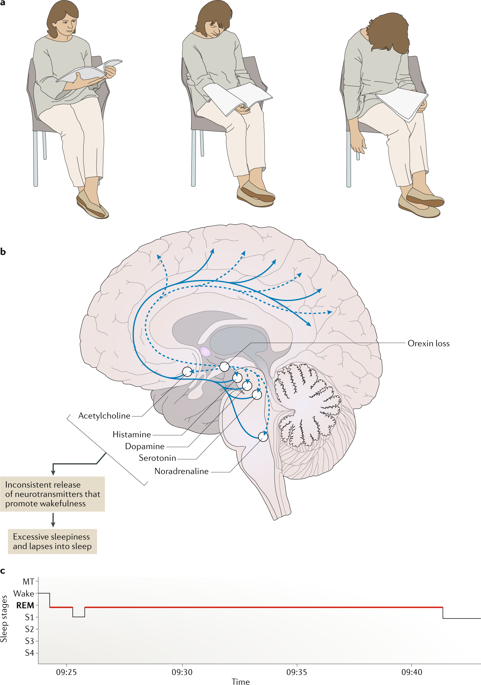
No triggering events (eg infection or vaccination) preceding the onset of symptoms were identified. Simultaneous with the development of EDS, the patient displayed daily cataplexy triggered by laughter up to several times a day. He was an active smoker, reported occasional alcoholic consumption, and denied any drug use. His medical history included right-shoulder surgery for multiple dislocations. He was working as an operator of construction machines and heavy goods vehicles. Case ReportĪ 35-year-old man began to experience excessive daytime sleepiness (EDS) with irresistible sleep attacks and involuntary napping, usually with two short (5–10 minutes) and refreshing naps in the afternoon. We describe the unusual case of a man with NT1 with a disease course that evolved towards the remission of narcolepsy symptoms at 15 years after disease onset, allowing termination of all treatments. Patients may experience an improvement in symptoms with advancing age, although a complete remission actually is a really uncommon phenomenon. 3 However, available treatment options are not disease modifying and NT1 is usually considered as a non-remitting chronic disease with a variable course over the years. 2 Pharmacological treatment of patients with NT1 relies mainly on stimulant and anti-cataplectic drugs. The main clinical features are severe, and include irresistible excessive daytime sleepiness (EDS), cataplexy, sleep hallucinations, sleep paralysis and fragmented nocturnal sleep. 1 NT1 is associated with a variety of sleep and wake symptoms. Narcolepsy type 1 (NT1) is considered to be a rare, lifelong neurological disorder related to selective loss of lateral hypothalamic orexin neurons due to a possible autoimmune process. Keywords: narcolepsy, cataplexy, excessive daytime sleepiness, orexin, hypocretin, remission However, spontaneous remission of disease occurred after 15 years.
During the first years after disease onset, the patient did not show any significant improvement despite treatment with a variety of stimulant and anti-cataplectic drugs. Université de Paris, NeuroDiderot, Inserm, Paris, F-75019, FranceĪbstract: We describe the case of a male patient who was diagnosed with narcolepsy type 1 on the basis of sleep and wake symptoms, and the results of investigations including video-polysomnography, multiple sleep latency test, human leukocyte antigen status and orexin level in cerebrospinal fluid.
Geoffroy Vellieux, 1, 2 Justine Frija-Masson, 1, 2 Anny Rouvel-Tallec, 1, 2 Xavier Drouot, 3 Marie-Pia d’Ortho 1, 2ġUniversité de Paris, NeuroDiderot, Inserm, Paris, F-75019, France 2Centre du sommeil, Service de Physiologie – Explorations Fonctionnelles, AP-HP, Hôpital Bichat-Claude Bernard, Paris, F-75018, France 3Neurophysiologie Clinique et Explorations Fonctionnelles, CHU de Poitiers, Poitiers, France


 0 kommentar(er)
0 kommentar(er)
